Software
Revenue Performance Advisor
An end-to-end revenue cycle management software solution for physician practices, labs, home health, medical-billing services, and other providers that want to help simplify workflows, reduce denials, optimize revenue, and improve patient engagement.
What’s Included in Revenue Performance Advisor
Optimizeyour revenue cycle from patient check-in to payment posting

Help increase upfront collections and gain workflow efficiencies
Revenue Performance Advisor prompts timely payments by providing patients with easy-to-understand estimates of their payment responsibility and multiple payment options, prior to care.
Plus, our solution simplifies management of rejections and denials by performing real-time edits, accessing a library of templated appeal letters, and resubmitting claims within minutes.


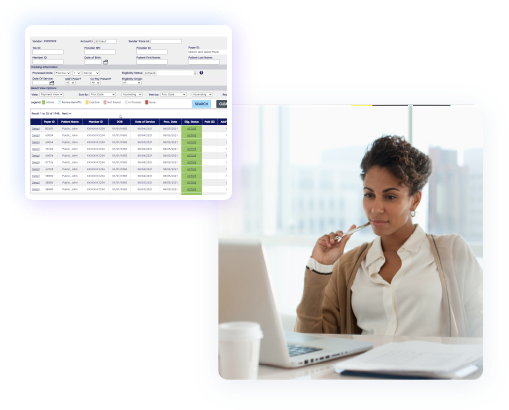
Help reduce denials and gain insights into practice performance
Streamline eligibility and benefits verification by accessing our expansive network of payers for the most up-to-date information.
Also, Revenue Performance Advisor can help identify problematic trends before they negatively impact practice profitability by using our advanced reporting capabilities.

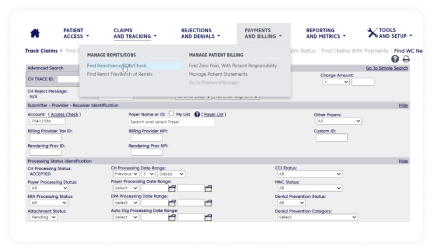
Easily submit, track, and manage claims
Help reduce rejections by using Revenue Performance Advisor to validate and scrub claims before submission. We have a first-pass clean claims rate of up to 99%.

Speed submissions and cut costs
End the time and labor drain of scanning, mailing, and faxing by attaching documents digitally. Benefits of streamlined attachment include faster adjudication and reimbursement, faster responses to payer document requests, and reduced risk of denials.
Our outcomes
PRODUCT SUPPORT
Need support for
this solution?
- Clearance Estimator Learn how we can help you create better patient estimates at or before the point of service to help increase collections and improve patient satisfaction. Learn more
- Coverage Insight Discover our analytics-driven solution for identifying undisclosed coverage for self-pay or underinsured patients, while adhering to anti-phishing regulation. Learn more
- Financial Counseling See how our eligibility and financial clearance services help decrease uncompensated care by helping patients find appropriate funding sources for medical bills. Learn more
Join revenue cycle management discussions
Find and share knowledge, exchange ideas, and collaborate with peers to drive your Change Healthcare solutions to success.