Solution Bundle
Claiming and Remittance
A claiming and remittance solution for payers, providers, and TPAs who want a smarter, more efficient, paperless solution to accelerate the healthcare revenue cycle.
What's included
Optimizeclaims and remittance processing

Fast, secure payments with seamless integrations
Facilitate faster and more accurate processes with digital transactions, configurable edits, and cloud-based solutions by using our latest technology innovations.
Get more from APIs and security and compliance tools by using flexible solutions that integrate seamlessly with your applications.

Leverage direct connections
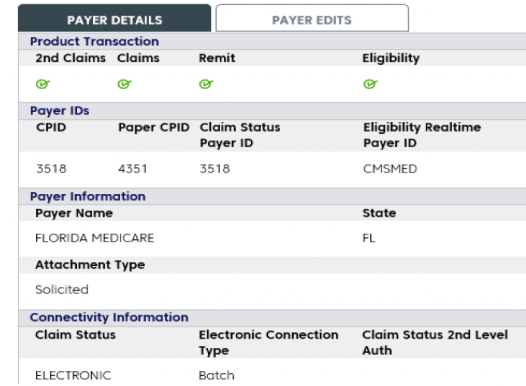
Help ensure that transmitted claims and remittances reach their final destinations transparently, quickly, and accurately by using our direct connections with payers, providers, labs, and pharmacies.

Accelerate the revenue cycle and maintain visibility of your transactions
Help reduce payment and transaction processing delays by enabling intelligent alerts and dashboard views, so you can proactively address problems, opportunities, and trends.
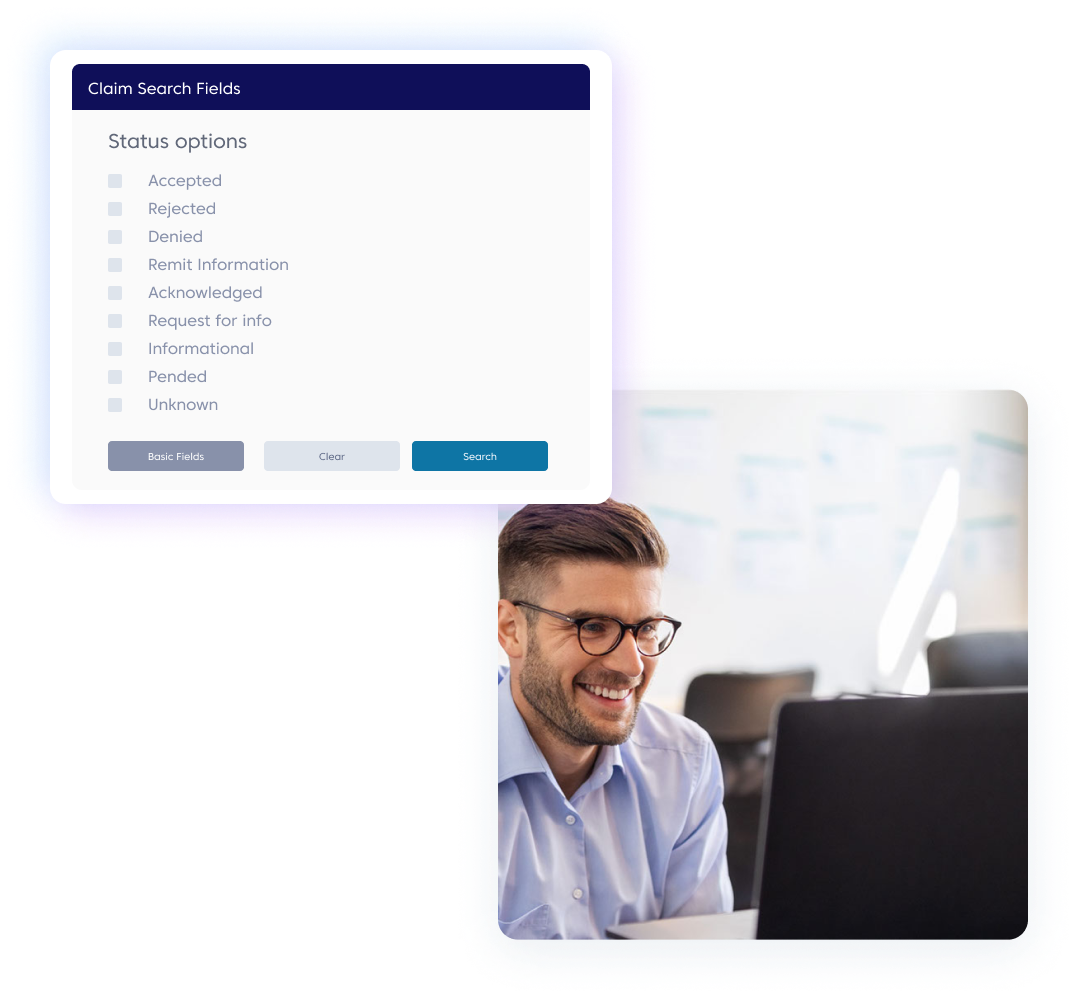
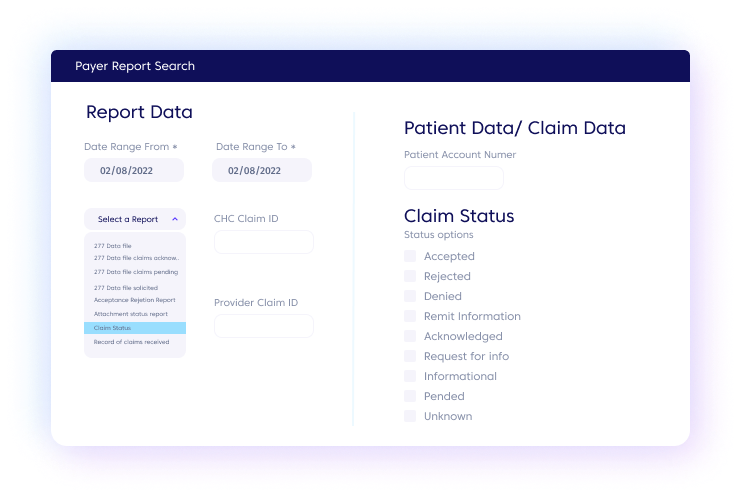
Get instant access to 15 months of data and multiple export options by using flexible search options, including patient, payer, batch, and status queries.
Our outcomes
PRODUCT SUPPORT
Need support for
this solution?
Mammography Software That Accelerates Your Healthcare Transformation

An electronic claim attachments solution for providers, payers, and partners who want to eliminate manual processes to improve revenue cycle efficiency.
Eligibility & Patient Access

A patient access solution for providers and payers who want to improve claim accuracy and help support timely, appropriate care with access to real-time eligibility and benefits verification and authorization requirements.
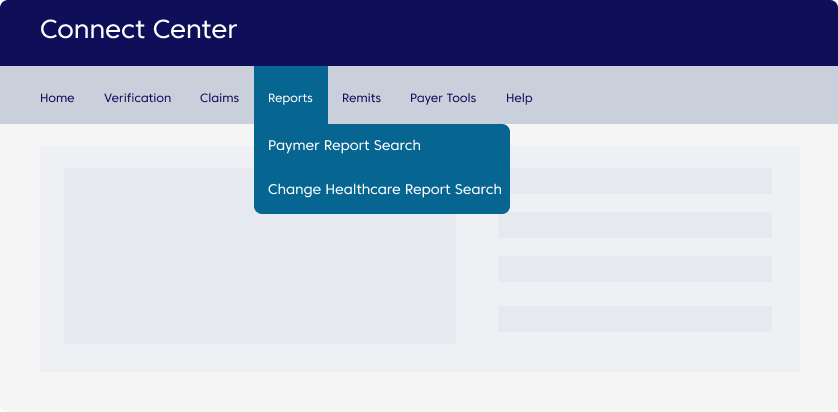
ConnectCenter™
A medical claims management solution for providers who want to improve claim accuracy, streamline submissions, and optimize denials-and-appeals management.
Claims Automation

A state-of-the-art solution for payers that want to outsource full or partial mailroom operations, including scanning, imaging and data capture, in order to streamline processes and focus on core business competencies.
Join Community discussions
Find and share knowledge, exchange ideas, and collaborate with peers and Change Healthcare experts to drive your solutions to success.

